SADO HIV / AIDS CARE AND SUPPORT PROGRAM.

🎯 Activity Title:
Increase Demand and Access to Quality HIV/AIDS Health Care Services
📌 Objective:
To empower vulnerable populations—especially people living with HIV (PLHIV), orphans and vulnerable children (OVC), adolescent girls and young women (AGYW), and key populations (KPs)—to actively seek, access, and utilize quality HIV/AIDS prevention, treatment, and care services, thereby improving health outcomes and quality of life.
🧩 Key Components of the Activity:
1. Community Sensitization & Health Education
- Conduct targeted HIV/AIDS awareness campaigns to address stigma, myths, and misinformation.
- Use radio, drama, community meetings, peer-to-peer education, and social media to reach underserved and at-risk groups.
- Focus on rights-based messaging to build confidence in using available services.
2. Peer-led Demand Creation Initiatives
- Train HIV-positive peers, adolescent champions, and community health workers (CHWs) to act as HIV ambassadors.
- Empower peer educators to conduct outreach in informal settlements, schools, refugee camps, and rural areas.
- Organize community dialogues and experience-sharing forums to promote positive living and reduce internalized stigma.
3. Integrated Health Outreach Services
- Take services closer to the people through mobile clinics and community health days offering:
- HIV testing and counseling (HTS)
- ART initiation and refills
- Viral load testing
- PMTCT and SRHR services for women and girls
- Combine HIV services with nutrition, NCD screening, and gender-based violence (GBV) services to make access easier and holistic.
4. Linkage and Retention Support
- Strengthen referral systems using CHWs and case managers to ensure that those who test positive are quickly linked to care.
- Establish adherence clubs, youth-friendly clinics, and community ART groups (CAGs) to improve retention in care.
- Support home visits and follow-up for defaulting clients, especially in hard-to-reach or rural areas.
5. Addressing Structural Barriers
- Work with local leaders, religious leaders, and opinion influencers to create supportive environments for PLHIV.
- Train health workers on non-discriminatory, gender-sensitive, and youth-friendly service delivery.
- Support programs that address transportation, food insecurity, and legal protection, which often prevent access to care.
Other Objectives
- Increase demand and Access to quality HIV AIDS Health Care Services.
Improve availability and uptake of HIV prevention, testing, treatment, and care services particularly among vulnerable and underserved populations through targeted outreach and inclusive service delivery models.
- Improve utilization, Retention and Adherence to ART through Affordable and Sustainable Access to ARVs and food therapeutics.
Partnership with National and International Development agencies and Pharmaceutical Companies to increase access to quality ART through local insurance schemes, grants ,
Strengthen supply chain systems and community-level support to ensure consistent, affordable access to quality-assured antiretroviral drugs and promote long-term treatment adherence.
- Strengthening Community-Based Support Networks and Referral pathways. Enhance and expand community-led structures and multi-secretarial referral pathways to ensure timely identification, linkage, and follow-up of people living with or affected by HIV/AIDS.
- Integrate Food and Nutrition Support into HIV/AIDS Care and Treatment.
Using food as Nourishment and Therapy ( Food Based Approach )
- Strengthen HIV -AIDS Data Management and Digitalizing Reporting Systems Pilot Digital HIMIS Data management, modernize and strengthen the Health Management Information System (HMIS) through digital tools, capacity building, and real-time data reporting to improve program monitoring, decision-making, and future programming.
🧒🏽👵🏼 Target Population:
- Vulnerable PLHIV (e.g., women, adolescents, elderly)
- Key populations (sex workers, men who have sex with men, people who inject drugs)
- Orphans and vulnerable children (OVC)
- Pregnant women and lactating mothers (for PMTCT)
- People in rural or refugee-hosting communities
📈 Expected Outcomes:
- Increased uptake of HIV testing and counseling (HTS) services
- Early initiation and consistent adherence to ART
- Improved viral suppression rates among PLHIV
- Reduced HIV-related stigma and discrimination in communities
- Strengthened linkage between community and health facility-based services
💡 Why This Matters:
Many vulnerable individuals face barriers to accessing HIV services, including stigma, misinformation, poverty, distance to health facilities, and lack of youth-friendly or gender-sensitive services. By increasing demand and improving access to quality, person-centered HIV care, this activity supports:
- Better health outcomes
- Reduced HIV transmission
- Empowered communities and individuals

Integration of Non-Communicable Diseases (NCDs) into HIV Services in Uganda
Background Uganda is experiencing a growing dual disease burden of HIV and Non-Communicable Diseases (NCDs), particularly among PLHIV who are living longer due to expanded access to ART. Common NCDs in this population include hypertension, diabetes, cervical cancer, and mental health disorders. The Ministry of Health (MoH), in alignment with global and national strategies, has prioritized integrating NCD prevention, screening, and management into HIV service delivery to ensure a holistic, person-centered approach to care.
Policy and Strategic Direction – The National HIV/AIDS Strategic Plan (2020/21–2024/25) explicitly supports the integration of NCD services into HIV programs. MoH included NCD management in the Revised Consolidated Guidelines for Prevention and Management of HIV (2022), and added NCD indicators to the revised Health Management Information tools.
Implementation Highlights – Capacity building for HIV service providers, including Community cadres, through in-service training, mentorship and task-shifting on NCD management. Provision of NCD data management and screening tools, job aides, IEC materials, diagnostics and medicines. Integration of NCD screening and treatment into routine HIV prevention and treatment visits and programs.

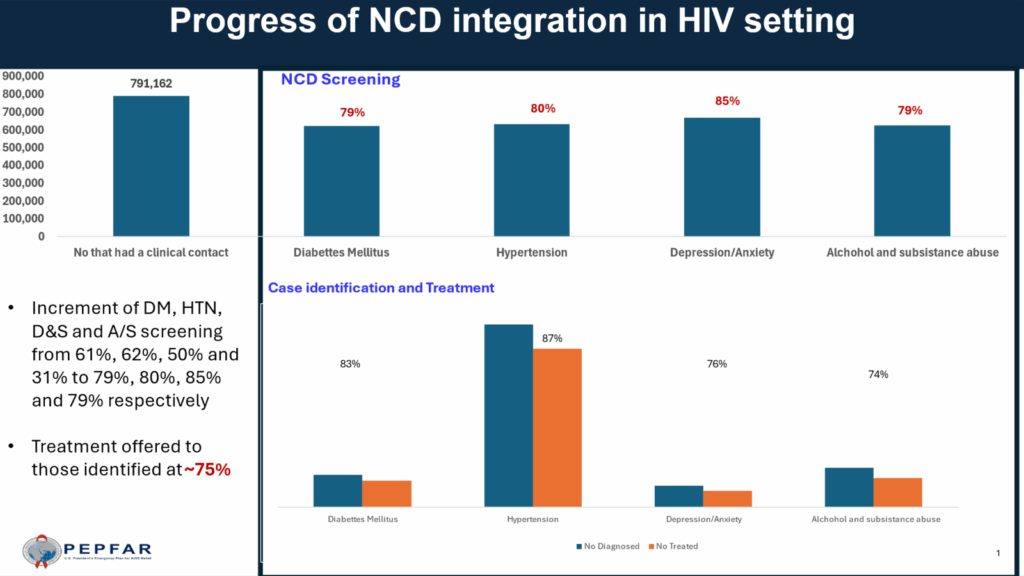
Performance Data FY 2025 Quarter 2 (Jan -March 2025)-highlights
- Increment of Diabetes Mellitus, Hypertension, Depression & Anxiety and Alcohol and /Substance abuse screening from 61%, 62%, 50% and 31% to 79%, 80%, 85% and 79% respectively, compared to Quarter 1,
- Treatment offered to those identified averaged at ~75%
Challenges:
- Limited resources and capacity to support full integration, including diagnostics and medicines
- Inconsistent data capture in DHIS2 and EMR systems for NCD indicators among PLHIV
- Gaps in provider knowledge and confidence in managing NCDs
- Low levels of community awareness about NCDs
- Fragmented funding streams for HIV and NCDs, leading to vertical programming and operational inefficiencies
Opportunities and Recommendations – Leverage the existing HIV infrastructure for broader NCD screening, prevention and management. Institutionalize integrated service delivery packages across all ART sites and in the out- and in-patient service delivery points, in line with the current MOH direction. Strengthen healthcare systems, including leveraging public-private partnerships: infrastructure, human resources, and essential medicines and technologies for diagnosis, treatment, and monitoring. Improve early detection. Strengthen community-based programs, awareness, linkages and referral.
Conclusion Uganda has made commendable strides toward integrating NCD care into HIV services. However, targeted investments, improved data systems, and continued health system strengthening are essential for sustainable scale-up. Addressing NCDs among PLHIV is critical for achieving optimal health outcomes and enhancing the resilience of Uganda’s healthcare system.
Annexes-FY 2025 Quarter 2 (Jan -March 2025) performance—details (Source-PEPFAR)